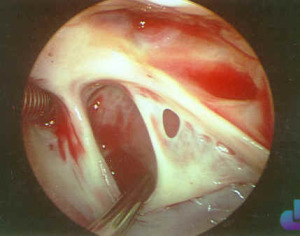
Atrial septal defect (ASD) is an abnormal openning between the right atrium and the left atrium (Figure). There are several types of ASD:
- Secundum ASD, the most common type (80% of cases)
- Sinus venosus type, which is almost always associated with anomalous drainage of the right upper pulmonary vein into the superior vena cava
- Ostium primum type, which is discussed with atrioventricular canal defects
- Other less common types of defect including coronary sinus septal defects and scimitar syndrome
Physiology
The direction of the blood flow across the ASD (shunt) is determined by the relative compliance of the right and left ventricles (relative stiffness of the ventricles). The left ventricle is usually less compliant than the right ventricle and therefore the flow is from the left atrium to the right atrium (left to right). The volume of blood in the shunt is determined by the size of the defect and the relative compliance of the ventricles. The volume of shunt is expressed as the ratio of blood flowing through the lungs (pulmonary blood flow) versus the volume flowing through the body (systemic blood flow). With a left to right shunt the volume of blood flowing through the lungs may reach three or four times the volume flowing through the body. If the relative compliance of the ventricles change, or the downstream resistance changes, left to right flow through the ASD can increase, decrease or actually reverse and become right to left (pulmonary blood flow becomes less than systemic blood flow)
Pathology
The increased blood flow through the right atrium, right ventricle and the lungs has several deleterious effects. These include increased workload for the right side of the heart which can lead to atrial and ventricular enlargement (dilatation) and unfavorable consequences such as arrhythmias (irregular heart beat). In addition, the increased pulmonary blood flow can lead to damage in the blood vessels in the lungs, which increases the resistance in the lungs and may lead to a right to left shunt with right ventricular failure (Eisenmengers syndrome). The life expectancy of patients with untreated ASD’s is markedly reduced.
Surgical Indications and Approach
The treatment of ASD is individualized for each patient. Symptomatic patients are usually treated as soon as symptoms develop. These may include shortness of breath, rapid breathing, difficulty feeding, poor weight gain or poor exercise tolerance. Asymptomatic patients with more than about a 50% increase in pulmonary blood flow are operated on electively, usually between two and four years of age.
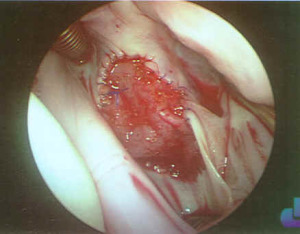
The surgical approach to ASD’s is to close them, either with a simple suture or a patch (usually of native material from the child). If other lesions are present (such as anomalous pulmonary venous drainage) they are repaired at the same time.
Surgical results are typically excellent, with very little or no mortality, morbidity (complications) or recurrence.